Overview
Claim Insight is a platform for working with medical claims.
Claim Insight parses claims in X12 EDI format, performs a number of checks to ensure claims correctness and makes claims available for analysis.
Claim Insight can quickly ingest a high volume of claims.
Claim Insight allows users to search claims and claims data elements, such as provider, patients and medical codes, by a number of different parameters, including names, addresses, identification numbers, code descriptions, patient’s age and medical conditions and many others.
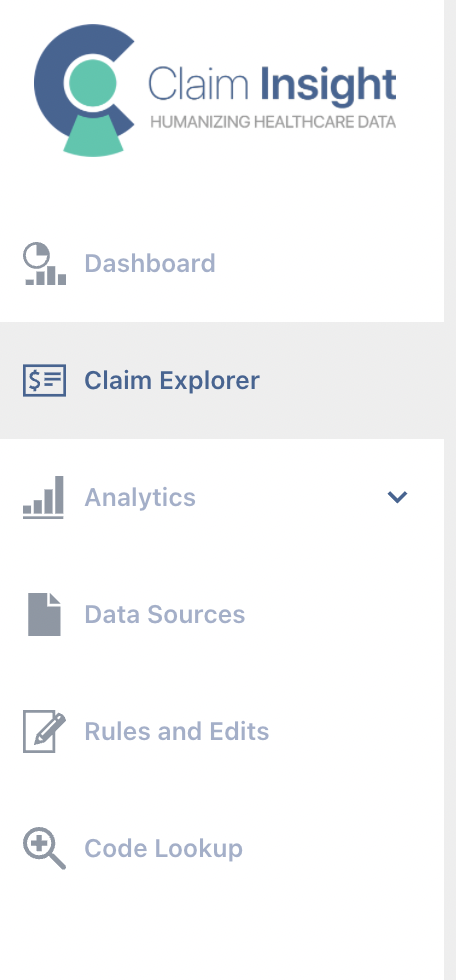
Claim Insight consists of the following key components:
- Claims and payments views. This is the UI for searching and viewing claims and payments.
- Analytics. Analytics views identify medical codes, providers, members, time intervals, locations and data quality issues based on various metrics, such as billed and paid amounts, claim and line counts and others.
- Data Sources. This is the UI for defining locations/sources of your X12 EDI and NCPDP files. Claim Insight “ingests” files from these sources and makes the data available for viewing and analysis.
- Rules and Edits. This is the UI for viewing and managing claim validation rules, such as Procedure to Procedure (PTP), Medically Unlikely Edits (MUEs) and others. Claim Insight supports so-called Medicare CCI coding edits and many additional rules.
The menu on the left provides access to these functions: